Introduction
Propofol is widely used intravenous anesthetics in clinical practice. Nevertheless, pain caused by propofol injection is unbearable for several patients. Propofol Injection Pain Ranked 7th in the most disturbing patient anesthetic experience.1Furthermore, among the 33 common anesthesia problems associated with outpatient surgeries, the frequency of pain caused by propofol injection was ranked third,2with an incidence as high as 90%.3During the induction of general anesthesia and sedation, some patients appear to be shouting, shrinking, and preventing arm action. Simultaneously, it can stimulate the body’s stress response, and the stress response can affect anesthesia induction and produce harm to patients, which is not consistent with the medical goals for anesthesia. The mechanism underlying injection pain associated with propofol has not been established. A study has suggested that it may be related to its composition; the water phase state and that the endothelium interact and stimulate the slow release of peptides, which induces the feel pain.4Several preliminary studies have investigated approaches to preventing or relieving propofol injection-related pain; these methods include non-drug approaches such as slowing injection speed,5choosing a thicker vein,6cooling the propofol,7dilution,8,9as well as drug interventions, such as the use of lidocaine,10opioids,11and nonsteroidal anti-inflammatory drugs.12,13Lidocaine pretreatment is the most widely used method for reducing propofol injection pain clinically.3However, lidocaine has side effects, such as allergy, contraindications, and safety risks related to blood coagulation function, which is a concern for the medical staff. To concurrently reduce the incidence of propofol injection pain and the side effects of lidocaine, we conceived combination therapy.14Transcutaneous electrical acupoint stimulation (TEAS) is a new therapy that combines Transcutaneous Electrical Nerve Stimulation (TENS) with traditional acupuncture therapy, which applies a specific density wave current to stimulate the human body.15This yields an effect similar to that of acupuncture and moxibustion, with subsequent analgesic effects.16,17Several clinical studies have shown that the analgesic effect of TEAS can be effective continuously, and it is not easy to lose the effect, and it has the advantages of being simple to administer, safe, and noninvasive.18–20It can also shorten the perioperative period in patients with inflammatory reactions, modulate immunity, and promote oxygenation, and it has been widely used in clinical research.21,22
Our previous studies confirmed that TEAS can alleviate propofol injection pain.16This study investigated the effects of TEAS combined with lidocaine on propofol injection pain. The purpose of this trial is to reduce the incidence of propofol injection pain and the severity of injection pain, observe its analgesic effect and whether it can reduce postoperative complications such as abdominal pain, bloating, nausea and vomiting, and promote faster and better postoperative patients. The rehabilitation of patients can provide a research basis for promoting the application of TEAS in the perioperative period of patients.
Materials and Methods
In this double-blind randomized control-group clinical trial, we studied the effectiveness of TEAS pre-stimulation combined with lidocaine in preventing propofol injection pain. A total of 220 women aged 18–65 years who were scheduled to undergo hysteroscopic surgery were enrolled in the study. All patients had a body mass index ranging from 18 to 31 kg/m2. Their American Anesthesiologists Society (ASA) grades were I or II. Furthermore, all patients provided written informed consent for elective hysteroscopy or surgical treatment. This study was conducted at The First Affiliated Hospital of Wenzhou Medical University, Zhejiang, China, from August 2020 to December 2020. All patients provided informed consent before participation. This prospective observational cohort study was approved by the Ethics Committee (2020–051) of the Clinical Research of the First Affiliated Hospital of Wenzhou Medical University and conducted in accordance with the Declaration of Helsinki. The Clinical Trial Number is ChiCTR2000036066.
Patients with a history of chronic pain syndrome, thrombophlebitis, neurological disease, forearm or thrombophlebitis syndrome with acute and chronic pain, severe mental illness, communication challenges, or digestive tract ulcers and those allergic to lipid medications, propofol, or general anesthetic drugs were excluded from the study. Patients allergic to lipid propofol, medications, and general anesthetic drugs; those with a history of analgesic or sedative drug use; and those who had a surgical incision, surgical scar, or skin infection at the Hegu and Neiguan acupoints, nerve damage in the upper extremities, or a history of spinal surgery were also excluded.
The visual analogue scale (VAS) is used for pain assessment. The basic method is to use a moving ruler with a length of about 10cm. One side is marked with 10 scales. The two ends are respectively “0” and “10” points. A point of 0 means no pain. A score of 10 represents the most severe pain that is unbearable.
The verbal rating scale (VRS). It consists of a series of adjectives used to describe pain, also known as the Verbal Evaluation Scale. The descriptive words are arranged in order of pain from the lightest to the strongest. There are 4 grades. VRS scores were categorized as follows: 0, no pain; 1, mild pain; 2, moderate pain; and 3, severe pain. If the score is greater than or equal to 2, the patient has obvious limb response. If the patient has no obvious physical reaction, we can ask the patient if he feels pain, and the score is 0 or 1. The method has been widely used to assess propofol injection-related pain.
The grade is divided into 0–3 degree. 0 means no dysmenorrhea. 1 means that the pain is mild. 2 is moderate pain, the pain is continuous, which affects rest and daily life, and can be relieved with analgesics. 3 is severe pain, the continuous pain cannot be relieved without medicine.
The maximum score is 10 point, and patients can leave the hospital if they reach 9 point.
Index: (a) signs: 2, fluctuations in the preoperative level (20%); 1, fluctuations in the preoperative level (20–40%); 0, fluctuations in the preoperative level (40% or more); (b): 2, can determine the orientation and smooth gait; 1, determine the azimuth or smooth gait; 0, cannot achieve more than anyone; (c): 2, mild; 1, moderate; 0, severe; (d), mild; 1, moderate; 0, severe; (e) Surgical bleeding: 2, mild; 1, moderate; 0, severe.
The main observation indexes included the highest severity of propofol injection pain and the VAS score for pain (0–3: mild; 4–6: moderate; 7–10: severe) and pain grade (0: absent; 1: mild; 2: moderate; 3: severe) after propofol injection during anesthesia induction. The secondary outcome measures, hemodynamics (heart rate, blood pressure, and pulse saturation), were recorded before anesthesia induction and 1 min after propofol injection. The total doses of propofol and remifentanil, duration of surgery, and duration from withdrawal to recovery were recorded. Respiratory depression (SpO2less than 90%) and intraoperative body movements were recorded. The discharge scoring system (PADS) score; postoperative bleeding days; and the types and incidence of postoperative complications after anesthesia were also assessed. Pain, edema, inflammation, and anaphylaxis were observed at the injection site and TEAS-treated acupoints and monitored.
The patients had to fast and abstain from drinking, not undergo any other preoperative examination, and take other medications, and four groups of patients use the same equipment.
TThe patients from groups T and L+T were administered TEAS 30 mins before anesthesia induction by an anesthesiologist who was not involved in administering anesthesia or pain efficacy evaluation during anesthesia preparation (groups K and L did not undergo any processing). The anesthesiologist selected acupoints of LI4 (Hegu) and PC6 (Neiguan) on both hands of the patients, stuck the electrodes, and connected Han’s Acupoint Nerve Stimulator (Nanjing Jinan Xinsheng Technology, Jinan, Nanjing, China) capable of producing a dilatational wave with a frequency of 2/100 HZ, which is the maximum tolerable for patients receiving −1 mA of electrical stimulation for 30 mins.
A 22-gauge trocar was used to open the hand dorsal veins of the patients when the patient is in the preoperative preparation room. After the infusion channel was connected to the extension tube, 500 mL Ringer’s solution was infused through the channel, with an infusion speed of 20 mL/min. The surgeons were informed about the patients undergoing routine surveillance, including pulse oxygen saturation, noninvasive blood pressure, and electrocardiogram. Meanwhile, the patients were administered oxygen (4 L/min) via a nasal cannula. Anesthesia was induced by another anesthesiologist. The four groups received 5 μg sufentanil (Yichang Renfu, Yichang, Hubei, China) from the infusion channel. Patients from group K and group T received 2 mL of saline, while those from the L and L+T received 2 mL of 2% lidocaine. After 1 minute, all patients were injected with 10% propofol (AstraZeneca, Shanghai, China) (2 mg/kg) at a rate of 1200 mL/hour by using a micropump (Zhejiang University Medical Equipment Factory, Hangzhou, Zhejiang, China). All patients were asked about the pain score every 5 s until they lost their consciousness (the same questions were used for all of them). We record the pain score at each point. The surgery was commenced, and anesthesia was maintained by continuous infusion of propofol (4 mg/kg·h) and remifentanil (Yichang Renfu, Yichang, Hubei, China) (0.1 μg/kg·min) via a micropump.
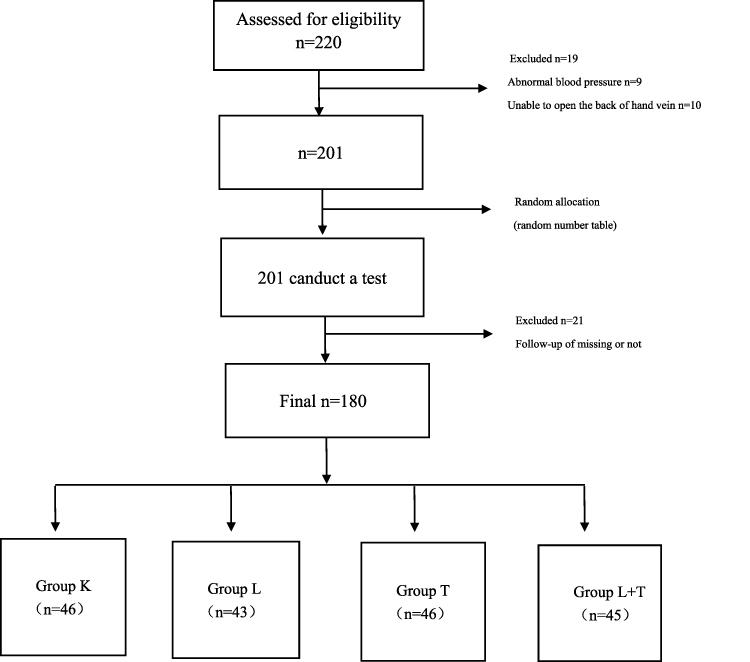
During the surgery, an additional single intravenous injection of 10% propofol (0.5 mg/kg) was administered if the patient physically responded to the surgical procedures, and the number of additions was recorded. If patiens’ mean arterial pressure (MAP) dropped below 60 mmHg, the patient received intravenous ephedrine (5–10 mg). And when their heart rate (HR) fell below 60 bpm, intravenous atropine (0.5 mg) was administered. Mask pressure oxygen was provided if their oxygen saturation (SPO2) fell below 90% (Figure 1). All drugs were preserved at room temperature and administered within 30 min of preparation.
Figure 1 Test flowchart. Abbreviations: TEAS, transcutaneous electrical acupoint stimulation; ECG, electrocardiogram; PADSS, discharge scoring system after anesthesia. |
In 42 pilot studies, the incidence of moderate to severe propofol injection-related pain decreased from 95% in the control group to 81% in the saline group (group K). With an α-value of 0.05 and a power of 0.8, the sample size of each group was determined to be 43. Taking into account the possible differences in venous access (hand veins, radial veins and cubital veins) and lack of follow-up, we set the sample size of each group to 55 people.
All data were analyzed using SPSS 25.0 (Statistical Product and Service Solutions, SPSS statistics is a statistical analysis software, which provides the core functions required to perform the whole process analysis). Randomization was performed using the random number method. The measurement data conforming to a normal distribution and homogeneity of variance were expressed as mean ± standard deviation. One-way analysis of variance was used for the intergroup comparisons. The LSD (Least—SignificantDifference) method was used for pairwise comparisons of data with statistically significant differences. Data that were not normally distributed were expressed as median (quartile spacing). The Kruskal–Wallis H-test was used. For the data that were significantly different across the groups, the LSD method was used for pairwise comparison of the rank orders. The statistical data were compared according to the sample size, theoretical frequency, and variable classification number and analyzed using the 2 test (or continuous correction 2 test or Fisher’s exact probability method). The rank data were analyzed using the Kruskal–Wallis H-test, and the ranks were compared using the LSD method. The test results were considered statistically significant at P<0.05.
Results
Of the 220 patients, 40 were excluded, including nine who reported abnormal blood pressure as they arrived in the operating room. These patients had no history of hypertension, but their systolic blood pressure (SBP) in the operating room was > 180 mmHg and did not decrease after 5 min. Moreover, 10 patients were excluded because the vein at the back of the hand could not be opened. The remaining 21 excluded patients refused to participate in follow-up trials after hysteroscopy or surgical treatment (Figure 2).
Figure 2 Recruitment flowchart numbers of patients recruited, the number of people excluded due to high blood pressure and the number of people missing from follow-up. |
There were no statistically significant differences in the general information, hemodynamics, and basic conditions of anesthesia operation among the four groups (P> 0.05) (Tables 1–3).
Table 1 Four Groups of Patients’ General Information |
Table 2 Four Groups of Patients’ Hemodynamics |
Table 3 Four Groups of Patients’ Basic Conditions of Anesthesia Operation |
The four-point verbal rating scale scores for propofol injection pain in the four groups were significantly different (P=0.010). There were statistically significant differences in the incidence of mild, moderate, and severe pain in the groups (P=0.012); the LSD results showed group L+T was significant differences in the incidence of injection pain from group K and group L (P=0.004, P=0.008). There were statistically significant differences in the incidence of mild, moderate, and severe pain among the different groups (P=0.012); the LSD results showed that group L+T was significant differences in the incidence of pain from K and T (P=0.007, P=0.037). The results showed that the combination of TEAS and lidocaine can reduce the incidence of injection pain and is more effective than single-use lidocaine (Table 4).
Table 4 Four Groups of Patients with Different Four-Point Verbal Rating Scale Information |
The VAS scores for propofol injection pain were significantly different among the four groups. There was a statistically significant difference in the pain severity across the groups (p=0.004). The LSD comparison results showed that there were statistically significant differences in pain between groups K and L, groups K and L+T (P=0.019, P=0.000). There were significant differences in the incidence of mild (0–3) or moderate (4–6) pain among the groups (P=0.015). The LSD comparison results showed differences in the incidence between groups K and L+T, groups L and L+T (P=0.003; P=0.011). The comparison showed that the TEAS and lidocaine combination can reduce propofol injection pain and is more effective than single-use lidocaine (Table 5).
Table 5 Four Groups of Patients with Different VAS Information |
The prevalence of nausea, vomiting, abdominal pain, and abdominal distension after surgery among the four groups were statistically different. There were no significant differences in the incidence of nausea and vomiting within 30 min after surgery. The incidence of nausea and vomiting at 24 hours after operation in the four groups was significantly different (P<0.05). The details are as follows. Compared with group L+T, the indexes of group K and L are statistically different (P<0.05). There was a statistically significant difference in the incidence of nausea and vomiting at 24 hours; compared with group T, group K and L had statistical differences (P<0.05). There was no statistically significant difference in the other groups (P>0.05). There was a statistically significant difference in the incidence of abdominal pain and bloating in the four groups at 30 min after operation (P<0.05). The details are as follows. Compared with group L+T, group L has statistically different indicators (P=0.001). There was no statistically significant difference in the other groups (P>0.05). There were statistical differences in the incidence of abdominal pain and abdominal distension at 24 hours after operation in the four groups (P<0.05). The details are as follows. Compared with group L+T, the indexes of group K and L are statistically different (P<0.05); compared with group T, group K and L had statistical differences in indicators (P<0.05), and the differences in the other groups were not statistically significant (P>0.05). TEAS can reduce the incidence of nausea, vomiting, abdominal pain and bloating in patients 24 h after surgery (Table 6).
Table 6 Four Groups of Patients with Different Nausea and Vomiting and Abdominal Pain and Abdominal Distension After Surgical Information |
The bleeding days after surgery were significantly different across the four groups (P<0.05). For groups T and L+T, the number of bleeding days after surgery significantly reduced relative to those for the other two groups. TEAS can shorten the duration of postoperative bleeding (Table 7).
Table 7 Four Groups of Patients with Different the Bleeding Days After Surgical Information |
Discussion
Propofol is among the most widely used intravenous anesthesia drug. However, pain caused by propofol injection is unbearable for several patients. Reducing the incidence and severity of propofol injection pain is an important clinical goal. A safe and effective method for preventing propofol injection pain or reducing its severity has not been established.
TEAS is a new therapy that combines TENS with traditional acupuncture therapy.15To reduce the incidence and severity of propofol injection pain, as well as the side effects of lidocaine, we adopted combination therapy; therefore, this study combined lidocaine and TEAS for pretreatment to prevent propofol injection pain.
In this study, the incidence of propofol injection pain in group K was 76%, compared to the meta-analysis in 2011 showed that 60% slightly higher incidence of group K.23A possible reason for this is that the participants were mostly young female patients. Kang et al and Lee et al, in their research results, show that the young women these two factors are high-risk factors of the propofol injection pain occurred.6,24Group K of VAS score average is the highest among the four groups. The prevalence of nausea, vomiting, abdominal pain, and abdominal distension after surgery were higher in group K than in groups T and T + L.
The incidence and severity of propofol injection pain reduced in group L relative to group K; this shows that lidocaine has a specific preventive effect against propofol injection pain, and it is consistent with the results of previous research. However, the incidence of postoperative nausea, vomiting, and abdominal pain in patients with abdominal distention did not differ significantly. In addition, group L had more bleeding days than group T and L+T. Several studies have reported the inhibition of blood coagulation by lidocaine by mainly inhibiting platelet function.25–27The underlying mechanism has not been established; however, it has been speculated that lidocaine affects platelet aggregation by altering the platelet membrane stability, and some studies suggest that it can also affect active substances in the plasma.28,29
In this experiment, we selected analgesic acupuncture points from LI4-PC6. LI4 is one of the four groups of essential points of the body, including the acupuncture points in the Yangming hand. Several domestic studies have shown that electrical stimulation in LI4 and PC6 acupunctures can have analgesic effects, promote to activate blood, and calm the nerves, among others. These studies have reported that TEAS stimulation after PC6 acupuncture in patients can reduce the incidence and severity of postoperative nausea and vomiting,30,31especially among female patients,32which is also consistent with our experimental results. In group T, the incidence of postoperative nausea, vomiting, and abdominal pain in patients with diarrhea was significantly lower than that in groups K and L, and the difference was statistically significant. The severity of injection pain in groups T and K also decreased, but it was not significantly different from that of group L, compared with the effects of TEAS and lidocaine. However, the number of postoperative bleeding days was reduced after TEAS pretreatment relative to that in groups K and L. The differences were statistically significant. TEAS can shorten the duration of bleeding after hysteroscopy in patients. The present study did not report on the effect of TEAS on postoperative bleeding in patients and the mechanism was not established. Further studies are warranted.
Based on the four-point verbal rating scale and VAS scores, the incidence and severity of propofol injection pain, as well as the incidence of postoperative nausea and vomiting, abdominal pain, and abdominal distension decreased in group L+T, compared with groups K and L. The number of postoperative bleeding days also reduced in group L+T, compared with groups K and L. Thus, for outpatient hysteroscopy or treatment of female patients before surgery, TEAS, which may involve LI4 and PC6 acupuncture on both sides, for 30 min and injection of lidocaine can reduce the incidence and severity of propofol injection pain and the incidence of postoperative nausea, vomiting, and abdominal pain in patients with abdominal distension. In addition, TEAS can shorten the duration of postoperative bleeding and speed up the patients with rapid postoperative recovery.
This study has limitations. We did not further explore the acupoint stimulation mechanism; at the same time, we did not follow patients with postoperative recovery. The study combined TEAS pretreatment with lidocaine to prevent and reduce propofol injection pain. This effectively reduced the incidence and severity of propofol injection pain and significantly reduced the number of women treated with hysteroscopy. The incidence of postoperative nausea, vomiting, and abdominal pain diarrhea were also reduced and the duration of postoperative bleeding was shortened.
The study found that TEAS is effective in preventing propofol injection pain and hope that it will be used more widely given its safety profile. Further research on its mechanisms and other benefits are encouraged. In effect, the analgesic effects of TEAS and its ability to minimize postoperative complications and promote rapid postoperative recovery of patients were assessed to provide insights into its usefulness for perioperative patients and foundations for future research.
Conclusion
TEAS pretreatment combined lidocaine can effectively reduce the incidence and severity of propofol injection pain; the number of women requiring hysteroscopy examination or treatment; incidence of postoperative nausea and vomiting and abdominal pain and distention; and shorten the duration of postoperative bleeding.
