Chronic obstructive pulmonary disease (COPD), a leading cause of morbidity and mortality worldwide1, is characterized by airways obstruction, dyspnea, and reduced exercise capacity. Unintentional weight loss and low body mass index (BMI) have been independently associated with increased mortality risk in COPD patients2,3. Importantly, differences in body composition, such as disproportionate loss of muscle mass, are associated with worse exercise capacity and health-related quality of life in patients with COPD4,5. Early and accurate detection of differences in body composition may facilitate timely institution of appropriate management, such as improved nutrition and pulmonary rehabilitation.
Body composition measurements can be ascertained using a number of methods. The dual X-ray absorptiometry (DXA) scan is currently the gold standard measure of body composition; however, DXA scan is costly, may only be available in limited settings, is time-consuming, and involves exposure to ionizing radiation. Other methods such as skinfold thickness, hydro-densitometry, and bioimpedance analysis (BIA) have been utilized as alternatives to the DXA scan to clinically measure body composition6,7. BIA devices offer rapid, non-invasive assessments of percent total body fat based on the determination of total body water content. Given the ease of obtaining BIA measurements relative to DXA, the majority of studies of body composition in COPD patients have been conducted using BIA. However, variability in the performance of different BIA devices in measuring body composition in patients with COPD exists, with limited data available on the accuracy of portable and handheld devices7,8,9.
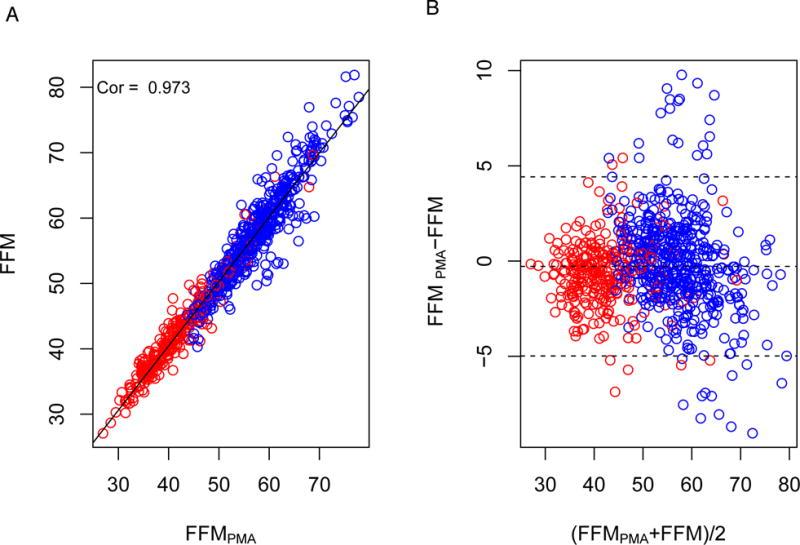
In the current work, we compared the accuracy of body composition measurements, including percent fat, fat mass, and fat-free mass, between the Omron HBF-306C (Omron Healthcare Inc., Bannockburn, IL, USA), a commercially available handheld BIA device that emits an extremely low electrical current of 50 kHz and 500 µA, relative to the DXA scan. The Omron HBF-306C BIA device provides measurement of percent total body fat, from which fat mass and fat-free mass (FFM) can be derived from concurrent anthropomorphic measurements (height, weight). For additional comparison, we determined FFM using anthropomorphic measurements alone (age, sex, height, weight) based on validated protocols10,11and compared the performance to DXA-assessed FFM.
In addition to our primary comparisons between BIA- and DXA-assessed measures of body composition, we performed several pre-specified secondary and subgroup analyses. First, because electrode placement can impact BIA measurements8,12, we examined the correlation between percent regional body fat measures (i.e., trunk, gynoid, android, arms, and legs.) obtained from the DXA scan and BIA device mean percent total body fat. Second, because the performance of BIA devices may vary at the extremes of BMI6, we compared the correlations (1) between BMI and DXA relative to BMI and BIA and (2) between BIA- and DXA-assessed body composition by obesity status.
