Alzheimer's disease (AD) is a progressive neurodegenerative disease and one of the most common causes of dementia with devastating morbidity and mortality1. AD is characterized by escalating cognitive decline, commonly anterograde amnestic cognitive impairments. Patients present with varying manifestations depending on the disease stage and primarily affected structures2. However, AD patients frequently present with deficits in recognition memory3, which notably can occur in prodromal stages as an early cognitive symptom4,5. Therefore, altered recognition memory is potentially associated with changes in regions' activities earlier than significant changes in volume or architecture, which could serve as biomarkers.
Several hypotheses have been introduced to explain the etiopathogenesis and clinical course of AD. The amyloid hypothesis is a widely accepted explanation based on extracellular aggregation and deposition of amyloid-beta peptides (Aβ) as a causal factor in AD6. The Aβ interferes with neuronal homeostasis, causes synaptic dysfunction and dysregulated neural excitability7, and triggers other pathological events8,9, leading to cognitive impairments. Compelling evidence demonstrated that cognitive impairment in AD might not be related to neuronal degeneration alone but also occur due to deficits in synchronized neural activities10,11. However, little is known about neural connectivity in circuits related to recognition memory.
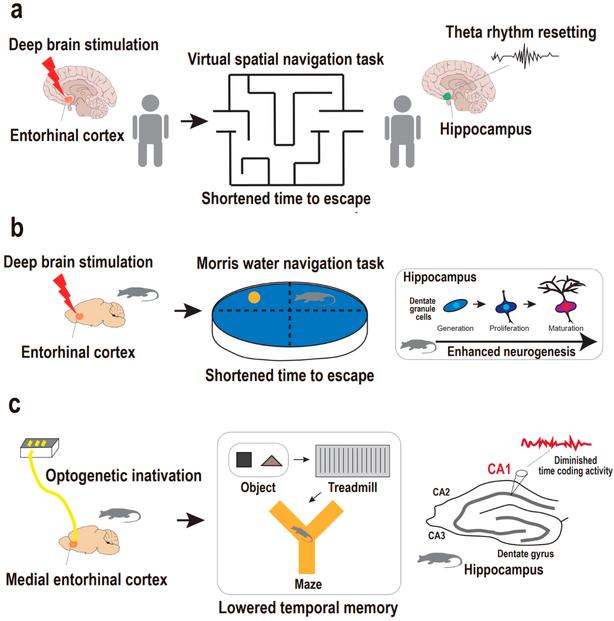
Organized communications and information transfer during memory processes in both local circuits and distant networks in the brain are allocated by synchronized rhythmic activities10. AD is associated with significantly disrupted connectivity in such neuronal communications12, which can be present from early preclinical stages before progression to overt Alzheimer's dementia13. Notably, AD tends to involve specific neural assemblies and networks that are more vulnerable to Aβ aggregates14. Two structures that are proposed affected in AD early stages are the entorhinal cortex (EC)15and hippocampus (HPC)16, both pivotal for proper memory functions, notably, object recognition17. Functional and structural changes in EC and HPC can be detected years before significant clinical symptoms, and therefore, suggested as potential biomarkers for AD diagnosis18.
Recent evidence indicates that olfactory network dysfunction may precede hippocampal formation damages19,20,21. Olfactory dysfunction is shown to be present as a disturbed sense of smell, proposed as an early sign of neurodegenerative diseases, including AD21. Functional changes in the olfactory system, particularly the olfactory bulb (OB), are shown in AD patients, with or even without smell problems21. Thus, OB can be a key candidate for investigating early functional changes in the brain induced by AD pathology.
Notably, the OB rhythmic oscillations, which are phase-locked to respiration, are global, propagate throughout the brain, coupled to fast cortical oscillations (e.g., gamma) and most importantly, synchronize distant regions' activities22,23,24,25. Therefore, OB could be considered a pivotal regulator of neural activity in the brain during cognitive performances26,27. On the other hand, the OB is closely connected with the EC-HPC circuit, which has synchronized oscillatory activity during spatial recognition22,28. Hence, exploring the OB network in recognition memory can provide useful information about dynamic functional connectivity alterations in AD.
The novel object recognition (NOR) task is widely accepted to evaluate memory deficits in AD animal models29. This task is based on the natural propensity of the animal to explore a new object, more than a familiar one, and does not concern spatial reference memory30. Given close structural and functional connections between OB and hippocampal formation, we hypothesized that the Aβ could disrupt OB-EC-HPC circuit connectivity in the AD rat model, resulting in recognition memory impairment. Therefore, to explore the circuit's connectivity in NOR performance, we simultaneously recorded local field potentials (LFPs) from OB, EC, and dorsal HPC (dHPC) during NOR task performance in an animal model of AD (Fig. 1 illustrates study protocol). This study can provide a better understanding of task-related dynamic circuit connectivity in AD, particularly in those regions that are more vulnerable to Aβ aggregates.
