In today's digitalized world, the incidence of obesity has been increasing to a point where negative consequences of obesity are witnessed in adults, especially in the younger generation [1], leading to a shorter lifespan. Obesity (body mass index (BMI) of 30 kg/m² or more) and overweight (BMI of 25 kg/m² or more) are known as abnormal or excessive fat accumulations that pose a health concern [2]. According to the global burden of disease recorded in 2017, four million people die each year due to being overweight or obese [3]. In the United States, obesity prevalence grew from 30.5% to 42.4% between 1999 and 2000. Simultaneously, the prevalence of extreme obesity increased from 4.7% to 9.2% [4].
Heart diseases, stroke, type 2 diabetes mellitus (T2DM), and perhaps certain types of cancer are all linked to obesity and are among the major causes of preventable early mortality [4]. Several comprehensive studies have shown an increase in mortality in patients who are above a specific BMI threshold, including impaired glucose tolerance, hypertension (HTN), cardiovascular disease (CVD), dyslipidemia, cerebrovascular disease, metabolic syndrome (MeS), pulmonary abnormalities, and gastrointestinal abnormalities [5].
Cardiovascular diseases are defined as the collection of disorders involving the heart and the blood vessels ranging from coronary artery disease (CAD), cerebrovascular disease, peripheral arterial disease, rheumatic heart disease, congenital heart disease, deep vein thrombosis, to pulmonary embolism. These CVDs are the major cause of mortality worldwide. In 2019, an estimated 17.9 million individuals died from CVDs, accounting for 32% of all global fatalities where myocardial infarction (MI) or a stroke caused 85% of these fatalities [6]. The risk of heart diseases could include an unhealthy diet, physical inactivity, tobacco use, harmful alcohol use, increased blood pressure/blood glucose/blood lipids, overweight, and obesity [6]. The risk of heart failure (HF) was examined across all cardiac diseases in the Framingham research, and the risk of HF was shown to be two-fold higher in the obese group than in the non-obese group [7]. There was a 9% increase in occurrences of ischemic heart disease for every unit change in BMI in the Asian Pacific Cohort Collaboration trial, which monitored over 300,000 people [5]. Due to the trending sedentary lifestyle and rampant increase in unhealthy diet, obesity is considered one of the dreadful risk factors for cardiac diseases that too considered an avoidable cause of death [3].
In order to tackle obesity, there are numerous regimes, including weight loss programs, diet, medications, surgeries, and devices such as electrical stimulation systems, gastric balloon systems, and gastric emptying systems [8]. Do bariatric procedures, when compared to other regimens, result in greater healthspan and restore an individual's overall quality of life in a reasonable amount of time?
Medical therapy that fails to achieve long-term weight loss is typical in people with severe obesity. Intense lifestyle modification can induce an average weight reduction of around 10% after one year and sustain weight loss of 5.3% after eight years [9]. The amount of weight lost varies greatly with each individual as it is a multifactorial approach; however, it has to be significant enough to control comorbidities [10]. According to emerging research, bariatric surgery can result in considerable weight loss and may also aid in the resolution of comorbid diseases, thus enhancing the quality of life [11]. The purpose of this review article is to emphasize the effects obesity may have on the cardiovascular health of an individual and whether bariatric surgery could benefit a patient in preventing cardiac complications, including premature death.
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines 2020 were followed in this systematic review [12], and the population, intervention, comparison, and outcome (PICO) format was incorporated in this study design.
Inclusion and Exclusion Criteria
The authors' inclusion criteria for this study comprised full-text reports within the past five years (2016-2021) published in the English language across the globe. The study population included human adults, both females and males, suffering from morbid obesity. One side of the group underwent bariatric surgery (intervention), and the other group received conventional treatment for obesity (comparison group) for a desirable overall health outcome. Only cohort and longitudinal studies were included for this research. All other articles before 2016, non-English language, non-full-text articles, and other study designs except those formally mentioned were excluded.
Information Sources, Search Strategy, and Data Extraction Process
A detailed search was done on databases mentioned above using the relevant keywords (disclosed below), and a total of 1,242 articles were identified. Two researchers worked independently to identify and extract data, as well as checked the quality of each study with appropriate quality appraisal tools from November 12, 2021, to November 22, 2021. After removing all duplicates, the reports were evaluated using the authors' inclusion and exclusion criteria, and any irrelevant reports were omitted, including those that did not meet the quality standards. In instances where there were disagreements, both researchers looked at the study designs, inclusion and exclusion criteria, intervention employed, and outcome assessment to come to an agreement. A third author was brought in to resolve differences and find a consensus in ambivalent circumstances. After a complete analysis, 10 reports were finally included in this review.
Keywords
MeSH keywords on PubMed are as follows: Bariatric surgery OR gastric bypass surgery OR weight loss surgery OR ("Bariatric Surgery/adverse effects" [Mesh] OR "Bariatric Surgery/complications" [Mesh] OR "Bariatric Surgery/ethics" [Mesh] OR "Bariatric Surgery/methods"[Mesh] OR "Bariatric Surgery/mortality" [Mesh] OR "Bariatric Surgery/therapy" [Mesh]) AND cardiac risk factors OR cardiovascular diseases OR ("Cardiovascular Diseases/abnormalities "[Mesh] OR "Cardiovascular Diseases/complications "[Mesh] OR "Cardiovascular Diseases/mortality "[Mesh] OR "Cardiovascular Diseases/prevention and control "[Mesh]). Keywords on other databases are as follows: Bariatric surgery; obesity; cardiovascular complications; risk factors; quality of life; gastric bypass surgery; premature cardiac death.
Quality Assessment
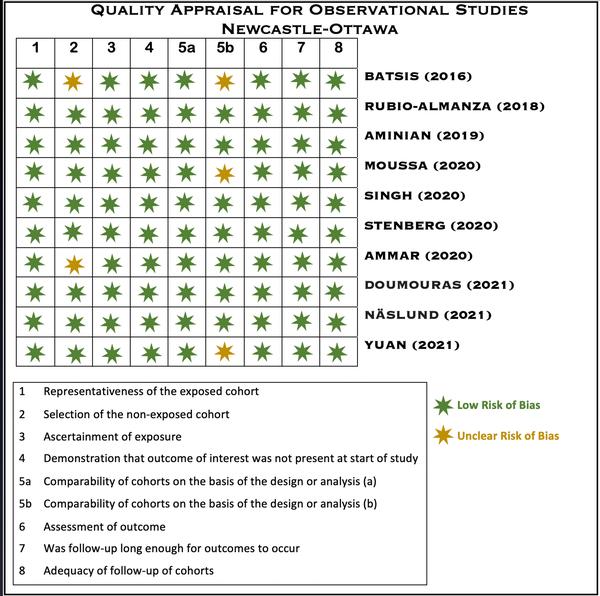
Figure 1 depicts the risk of bias assessed for the included studies by the Newcastle-Ottawa quality appraisal tool.
Figure1:Newcastle-Ottawa Quality Appraisal Tool for Observational Studies
Among the 1,242 articles, 698 were duplicates and were removed using EndNote (Clarivate Analytics, Philadelphia, United States), 64 were removed due to ineligible records, and 256 were removed for other reasons. A total of 224 records were reviewed, with 181 being discarded due to relevancy and inclusion/exclusion criteria, and 17 reports could not be retrieved. The final screening reduced the number of reports to 26, which were evaluated for quality and eligibility. After a thorough reading, the final eligible reports included 10 studies. The study did not use any automation tools. Figure 2 depicts the search process used for this review in the form of a PRISMA flow diagram [12].
Figure2:PRISMA Flow Diagram
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analysis.
Table 1 summarizes the conclusion of all included studies in this review.
| Author | Country, Year | Type of Study | Number of Subjects | Type of Bariatric Surgery | Conclusion |
| Batsis et al. [13] | United States, 2016 | Retrospective cohort | 40 | RYGB | Bariatric surgery causes significant weight loss, reduces cardiovascular risk factors, lowers MeS prevalence, and is an effective treatment in obese elderly patients (>60 years). |
| Rubio-Almanza et al. [14] | Spain, 2018 | Retrospective cohort | 105 | RYGB | In T2DM and prediabetes, bariatric surgery lowers the risk of CVD. |
| Aminian et al. [15] | United States, 2019 | Retrospective cohort | Exposed=2,287Control=11,435 | Adjustable gastric banding, duodenal switch, RYGB, and sleeve gastrectomy | There was a decreased risk of MACE among patients with T2DM and obesity who underwent metabolic surgery compared to the nonsurgical approach. |
| Moussa et al. [16] | United Kingdom, 2020 | Retrospective cohort | Exposed=3,701Control=3,701 | Not specified | Bariatric surgery lowers the long-term risk of severe cardiovascular events and acute HF in obese individuals. |
| Singh et al. [17] | United Kingdom, 2020 | Retrospective cohort | Exposed=5,170Control=9,995 | Duodenal switch, gastric banding, RYGB, and sleeve gastrectomy | Compared to standard care, bariatric surgery is linked to a lower risk of HTN, HF, and mortality; however, gastric bypass was linked to a lower incidence of CVD compared to standard treatment. |
| Stenberg et al. [18] | Sweden, 2020 | Cohort | Exposed=11,863Control=26,199 | Gastric bypass and sleeve gastrectomy | A lower incidence of significant adverse cardiovascular events, particularly acute coronary events, was associated with metabolic surgery. |
| Ammar et al. [19] | Egypt, 2020 | Longitudinal study | 100 | RYGB and sleeve gastrectomy | A beneficial improvement in cardiovascular risk profile, cardiac structure, and function was linked to weight loss. |
| Doumouras et al. [20] | Canada, 2021 | Retrospective cohort | Exposed=1,319Control = 1,319 | RYGB and sleeve gastrectomy | In individuals with cardiovascular disease and obesity, bariatric surgery minimized the risk of MACE. |
| Näslund et al. [21] | Sweden, 2021 | Cohort | Exposed=509Control=509 | RYGB and sleeve gastrectomy | Metabolic surgery is significantly associated with a lower incidence of serious complications, MACEs, mortality, new MI, and new-onset heart failure in highly obese individuals who have had a previous MI. |
| Yuan et al. [22] | United States, 2021 | Retrospective cohort | Exposed=308Control=701 | RYGB | Lower incidences of MACE were seen in patients with an early RYGB therapy for BMI reduction. |
Table1: Summary of Results From the Selected Studies
RYGB: Roux-en-Y gastric bypass; MeS: metabolic syndrome; T2DM: type 2 diabetes mellitus; CVD: cardiovascular disease; MACE: major adverse cardiac event; HF: heart failure; HTN: hypertension; MI: myocardial Infarct; BMI: body mass index.
Focal Points of the Included Studies
Batsis et al. [13]: One year following bariatric surgery, the prevalence of diabetes (57.5% to 22.5%; P<0.03), HTN (87.5% to 73.7%; P=0.003), dyslipidemia (80% to 42.5%; P<0.001), sleep apnea (62.5% to 23.7%; P<0.001), and MeS (80% to 45%; P<0.002) decreased. The baseline risk also decreased from 14.1% to 8.2% at follow-up [13].
Rubio-Almanza et al. [14]: The risk of cardiovascular disease in patients with T2DM and prediabetes was lower than the baseline risk (P=0.001) one year after surgery. BMI, body fat percentage, fasting plasma glucose (FPG), glycated hemoglobin A1C (HbA1c), c-peptide, homeostatic model assessment for insulin resistance (HOMA-IR), low-density lipoprotein cholesterol (LDL-c), systolic blood pressure (SBP), and diastolic blood pressure (DBP) lowered during the first year following the surgery. They had a flat trend or, in some cases, a very slight increase from the 12th to the 60th month. At 60 months, only 3.2% of the patients continued to have a high CVD risk, the remission from T2DM was 92%, and the prediabetic patients did not develop T2DM [14].
Aminian et al. [15]: The primary end-point had six outcomes: the first occurrence of all-cause mortality, coronary artery events, cerebrovascular events, heart failure, nephropathy, and atrial fibrillation. The secondary end-point outcomes included three-component major adverse cardiac event (MACE) (myocardial infarction, ischemic stroke, and mortality) plus the six individual components of the primary end-point. By the end of the study period, 385 patients in the surgical group and 3,243 patients in the nonsurgical group experienced a primary end-point (cumulative incidence at eight years; P<0.001) and an eight-year absolute risk difference [ARD] of 16.9%. All secondary outcomes, including mortality, demonstrated statistically significant differences in favor of metabolic surgery [15].
Moussa et al. [16]: Major adverse cardiovascular events were considerably less common in patients who had undergone bariatric surgery (P=0.001), which was primarily due to a decrease in myocardial infarction (P=0.001) rather than an increase in acute ischemic stroke (P=0.301) in addition to a reduction in new-onset HF (P=0.026) and mortality (P=0.001) [16].
Singh et al. [17]: In terms of combined cardiovascular risk factors, bariatric surgery, on the whole, was not significantly associated with lowering the risk factors; however, Roux-en-Y gastric bypass (RYGB) had a statistically significant association with the combined CVD risk factor (P=0.003). The all-cause mortality (P=0.004), hypertension (P<0.001), and heart failure (P=0.033) were all significantly lower in patients who underwent bariatric surgery regardless of the type of the surgery. These outcomes were similar in patients with T2DM and without T2DM, with the exception of atrial fibrillation, which was reduced in the T2DM group [17].
Stenberg et al. [18]: The primary outcome was a MACE, defined as the first acute coronary syndrome (ACS), cerebrovascular incident, fatal cardiovascular event, or unattended sudden cardiac death. MACEs were reported in 379 operated patients (3.2%) and 1,125 control subjects (4.5%). After controlling for hypertension, comorbidities, and education, the metabolic surgery group had a lower risk (P<0.001). When compared to controls, the surgical group had a lower risk of ACS events (P<0.001) and cerebrovascular events (P=0.060). The study's significant deficiencies were the absence of information on BMI and smoking history in the control group besides the nonrandomized study design [18].
Ammar et al. [19]: BMI, heart rate, blood pressure, diabetes, dyslipidemia, and, therefore, metabolic syndrome and Framingham risk score decreased significantly (P=0.0001) six months after surgery. HTN was 24% vs. 12% (P=0.0005), diabetes was 21% vs. 11%, (P=0.002), dyslipidemia was 32% vs. 7% (P<0.0001), and MeS was 54% vs. 26% (P=0.0001). Substantial improvement was seen in all lipid subfractions, and considerable reduction was evident in FPG, two-hour postprandial plasma glucose (2hPPPG), HbA1c, and liver enzymes. Weight loss with bariatric surgery was correlated with a significant reduction in resting heart rate and a shortening of the corrected QT (QTc) interval (P=0.009), which is a predictor of ventricular repolarization. In addition, echocardiographic findings at six-month follow-up revealed a significant reduction in left ventricle (LV) dimensions and LV mass index (LVM) (P<0.0001), a significant increase in left ventricle ejection fraction percentage (LVEF%) (P=0.0003), and an increase in early to late mitral inflow velocity (E/A) ratio (P<0.0001). Age, Framingham risk score, and preoperative BMI had substantial positive correlations with BMI at follow-up [19].
Doumouras et al. [20]: The primary outcome occurred in 11.5% of the surgical group (151/1,319) and 19.6% of the controls (259/1,319) (P<0.001). The association was well defined in individuals with heart failure (P<0.001; absolute risk difference, 19.3%) and ischemic heart disease (P<0.001; absolute risk difference, 7.5%). Surgery also showed a decrease in the risk of the secondary outcome, namely, myocardial infarction, ischemic stroke, all-cause mortality (P=0.001), and cardiovascular mortality (P=0.001) [20].
Näslund et al. [21]: Patients who underwent metabolic surgery had a decreased eight-year cumulative risk of MACEs (18.7% vs. 36.2%), reduced risk of death, and new-onset heart failure, but failed to detect significant changes in stroke or new-onset atrial fibrillation [21].
Yuan et al. [22]: The RYGB within one year (RYGB-1Y) group showed a decreased rate of MACE (P=0.008) and reduced mortality (P=0.04) than the No-RYGB group; however, the RYGB-1Y surgery was not significantly associated with lower atrial fibrillation occurrence (P=0.11) [22].
