Introduction
Pressure ulcers are an important indicator of hospital care quality1and a costly complication of intensive care.2Despite numerous studies on the causes of PU development, PU remain a major problem in hospital settings.3According to a 2017 report by NPUAP, each year 2.5 million patients in the US develop PU and 60,000 die from their complications as a result of inadequate treatment. A review of epidemiological studies comparing the prevalence and incidence of PU in Europe, USA and Canada found that the reported prevalence of PU in European hospitals ranged between 8.3% and 23%.4In the UK, the prevalence of PU in care settings was estimated at 10.2%, whereas the prevalence of PU in the USA and Canada ranged between 12.3% and 33%.5,6It is estimated that in Poland PU affect over 500,000 patients. According to a study on the prevalence of PU in Europe, it is estimated that one in four patients in neurology wards and one in five intensive care unit patients will develop PU.7PU are a global issue and a burden to patients and the healthcare system. The development of pressure ulcers in hospital settings is associated with increased length of hospital stay and increased treatment costs. According to a report by the Centres for Medicare & Medicaid Services, the costs associated with treating hospital-acquired PU in US patients amount to USD 146 million a year.8The identification and analysis of as many causes of the condition as possible would improve treatment effectiveness and reduce healthcare costs. There are significant differences in the prevalence of hospital-acquired pressure ulcers between intensive care units and other types of wards. This reflects the impact of critical illness on pressure ulcer development.9Intensive care treatment involves the use of respirators, urinary catheters and multiple intravenous catheters as well as the use of analgesics, muscle relaxants and sedatives, which cause a reduction in sensory perception, leading to a reduced reaction to pressure.10They may create additional health complications for the patient.11Pressure ulcers can be a source of infection and have a negative impact on the patient’s mental and physical health.12Hospital-acquired pressure ulcers may contribute to increased mortality. Low pressure ulcer prevalence is a marker of good quality of health care.9The incidence of PU is influenced by individual patient factors and the type of treatment used.6Numerous risk factors for PU have been identified in current research, including critical illness, older age, prolonged length of hospital stay, immobility, tissue hypoperfusion, poor nutrition, poor skin condition, being female as well as obesity.13–18Scientific publications have confirmed that there is an association between increased pressure ulcer risk and endogenous factors such as anaemia, decreased albumin levels, MAP <60-70 mmHg, diabetes, and the age of the patient.10,19–22Intraoperative and perioperative factors that have been found to be associated with pressure ulcer development include anaesthesia, duration of surgery, surgical position, and the postoperative bed used.23–25There are also studies that have found that the use of blood products during surgery is associated with the development of postoperative pressure ulcers.26Other external risk factors for pressure ulcer development include the duration of stay in the hospital, mechanical ventilation, hemofiltration, haemodialysis and the use of vasopressors.2,10,27,28
Table 1 Characteristics of the Groups Studied Calculated for Minimum Lactate Levels |
Table 2 Characteristics of the Groups Studied Calculated for Maximum Lactate Levels |
Patients after surgery have been shown to have reduced albumin levels and elevated blood lactate levels.29Lactate levels may be increased in many pathological conditions. The monitoring of lactate levels allows for the detection of an existing or imminent critical illness. Lactate is a product of anaerobic glycolysis that may cause severe metabolic disturbances. Increased lactate levels are associated with tissue hypoxia as well as increased morbidity and mortality.30–32
So far the impact of blood lactate levels on the development of pressure ulcers in intensive care unit patients has not been investigated.
The aim of the study was to establish the relationship between the incidence of pressure ulcers and blood lactate levels in intensive care unit patients.
Materials and Methods
The study was conducted among 125 patients (77 men and 48 women) treated at the Department of Anaesthesiology of the 4th Military Teaching Hospital in Wroclaw between October 2019 and March 2020. The patients included in the study were both patients after surgery and with internal diseases. The patients were divided into three main groups, which were each divided into two subgroups differing in blood lactate levels (subgroup A - patients with lactate levels within the normal range, subgroup B - patients with lactate levels above the reference range).
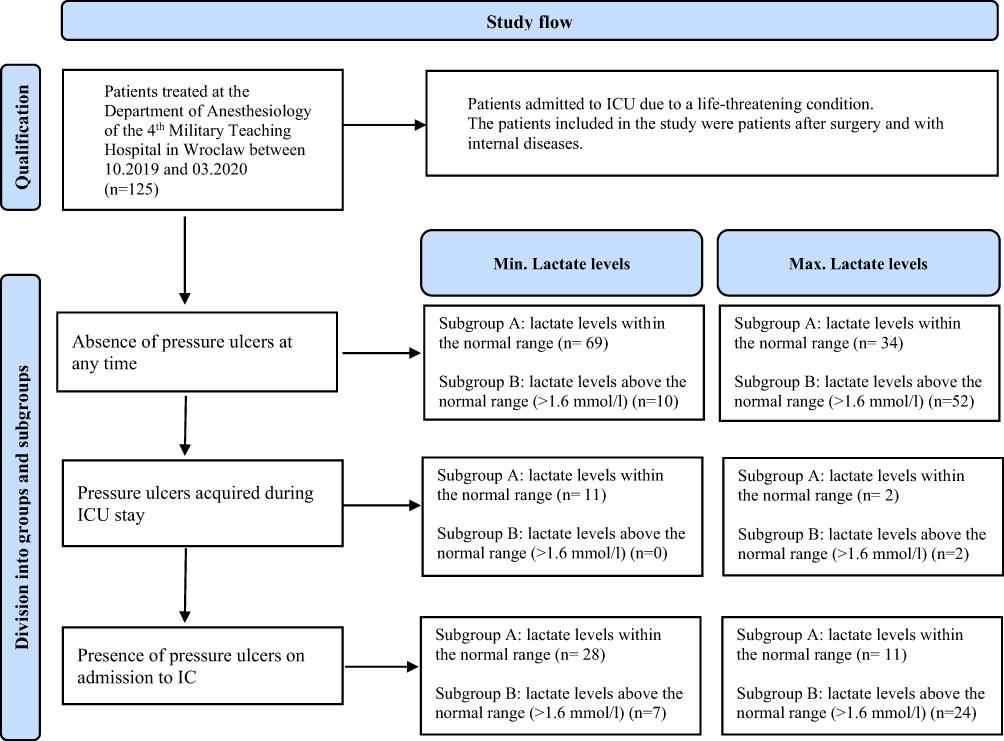
The first group included patients with no pressure ulcers on admission and at discharge. The second group included patients who had no pressure ulcers on admission but had pressure ulcers at discharge. The last group included patients with pressure ulcers on admission and at discharge. Lactate levels were measured by arterial blood gas analysis in each of the patients studied at least several times, with the minimum and maximum lactate levels in each patient being used for analysis (Figure 1).
Figure 1 Study flow. |
The criteria for inclusion in group one were as follows: the use of intubation, analgosedation and vasopressors, duration of stay in ICU of at least 48 hours, absence of pressure ulcers on admission and at discharge. The criteria for inclusion in group two were as follows: the use of intubation, analgosedation and vasopressors, duration of stay in ICU of at least 24 hours, pressure ulcers acquired during the patient’s stay in ICU. The criteria for inclusion in group three were as follows: duration of stay in ICU of at least 48 hours, presence of pressure ulcers on admission and the use of the treatment listed in criteria for inclusion in groups one and two.
This was a retrospective, non-randomised study. The study was approved by the Bioethical Commission at the Military Medical Chamber in Warsaw (No. KB - 186/21) and complies with the Declaration of Helsinki.
We analysed the patients’ lactate levels, as measured by arterial blood gas analysis, and monitored their pressure ulcers using their medical records: the pressure ulcer monitoring chart, the Waterlow pressure ulcer risk assessment chart, history of present illness and medical history. In the present study we used the study by Yepes et al investigating the relationship between pressure ulcer development and length of stay in ICU.33
The study group was compared with total Polish PU of the calculated incidence rate: 10.2 per 10,000 people. Statistical analysis was performed using the Statistica software. The χ2test of independence was used to test research hypotheses and examine the significance of differences for one degree of freedom (df). A level of significance of p = 0.05 was used in the study. Sample size calculation (confidence level: 95%, margin of error: 6%, population proportion: 12%, hospitalized population size: 327,000) resulted in 113 or more measurements in the study. Therefore, the study size seems to be suitable and adequate.
Results
The study was conducted among patients aged between 19 and 94 years. The mean age of the patients was 64.9 years, with similar mean ages for men (64.0) and women (66.5). The patients stayed in ICU for between 1 and 98 days, with the mean duration of stay of 11.5 days. The maximum length of stay in ICU was 98 days for male patients and 64 days for female patients. Lactate levels in the patients studied ranged between 0.2 and 30.0 mmol/l. There were 35 deaths during the study period.
Figure 2 shows gender-specific statistics regarding the age of the patients and the number of days they stayed in ICU. Lactate levels were measured in each patient by arterial blood gas analysis at least several times during their stay in ICU. Based on the results of the arterial blood gas tests, the minimum and maximum lactate levels for each subgroup were determined. An analysis of results was carried out based on two separate groups: for minimum and maximum blood lactate levels. The results are shown in Tables 1 and 2. Our analysis for minimum lactate levels showed that only 10 patients (8%) with no pressure ulcers had lactate levels above the reference range. The age range of the patients included in subgroup 1A (19–94 years) was similar to that of patients in subgroup 1B (20–87 years). Patients with no pressure ulcers and with low lactate levels stayed in ICU for between 1 and 64 days. There were 13 deaths in that group of patients. Our analysis showed that patients with lactate levels above the normal range and with no pressure ulcers stayed in ICU for between 1 and 7 days. Nine of those patients died. Subgroups 2A and 2B included patients who developed pressure ulcers while staying in ICU. In 11 (8.8%) of those patients’ lactate levels ranged between 0.2 and 1.5 and were considered to be within the reference range. The mean age of those patients was 68 years. The patients in the two subgroups stayed in ICU the longest, with the length of stay ranging from 4 to 98 days. Two of those patients died. All the patients who developed pressure ulcers during their stay in ICU had lactate levels within the normal range. Group 3A included patients with pressure ulcers on admission. Their length of stay in ICU ranged between 4 and 43 days and their lactate levels did not exceed 1.6. Five of those patients died. Six patients included in group 3B died and lactate levels in that group were above the reference range (1.7–12.9). The mean age of those patients was 64.3 years. The relationship between pressure ulcer development and blood lactate levels was tested using the maximum likelihood chi-square test. However, the test did not show a statistically significant relationship (p=0.1127). Our analysis for maximum lactate levels showed the following for group 1A, which included patients without pressure ulcers and with lactate levels within the normal range: age range of 19–94 years, duration of stay in ICU ranging from 1 to 26 days, 4 deaths; moreover, there were more men than women in that group. There were 19 deaths in group 1B, which included patients without pressure ulcers who had lactate levels above the normal range. Four patients (3.2%) developed pressure ulcers during their stay in ICU. There was one death in that group of patients. The third group included 35 patients (28%), of whom 11 had pressure ulcers on admission to ICU and had lactate levels within the normal range. Those patients stayed in ICU for between 4 and 20 days and were aged between 27 and 90 years. There were 11 deaths in group 3B, which included patients with high lactate levels (1.7–23.0) and with pressure ulcers on admission. The patients included in that group were aged between 52 and 89 years and stayed in ICU for between 1 and 43 days. The analysis was carried out using the maximum likelihood chi-square test to determine the relationship between lactate levels, as measured by arterial blood gas analysis, and the presence of pressure ulcers. The test did not show a statistically significant relationship (p=0.6148). Our study showed that the incidence of pressure ulcers in the intensive care unit patients studied is 8.8%, which is not statistically different to the incidence rates reported in the literature. According to the 2020 hospitalization report, about 327,000 patients are hospitalized in Poland. The median prevalence of PU in hospitalized patients is approximately 12%,4which means every year 39,240 people are at risk of developing a PU in Poland. The incidence rate measured for Poles is 10.2 per 10,000 people. We found that there was no difference in the incidence of pressure ulcers between the female and male patients studied. An analysis of the findings from the study did not show a clear association between blood lactate levels and the development of pressure ulcers due to low expected values. We suggest that further research on a larger population is required.
Figure 2 Descriptive statistics regarding the age and gender composition of the study participants, the number of days the patients stayed in ICU. |
Discussion
Elevated lactate levels can be observed in all conditions accompanied by significant hypoxia, such as shock, thrombosis, anaemia and acute respiratory failure, either of pulmonary or cardiovascular origin. They can be used in the diagnostic process as a sensitive prognostic factor with regard to the outcomes and treatment of patients. Sustained acidosis constitutes a pathological mechanism responsible for systemic inflammation, which leads to multi-organ failure. Metabolic acidosis also results in intensification of catabolic processes and systemic weakness caused by reduction in lean mass. Acidosis inhibits the synthesis of albumins and plays an indirect role in the development of heart failure as it inhibits the activities of Na+/K+-ATPase in heart muscle cells and red blood cells.34–36Lactate clearance in the body is dependent on the rate of oxidation in the relevant organs.37When liver perfusion decreases by 70% and renal perfusion decreases by 90%, the organs not only stop removing lactate but they also start to produce it themselves.38,39Numerous studies have shown that there is a link between lactate levels in the immediate postoperative period after cardiac surgery and both serious complications and postoperative mortality.30,40–47It has also been shown that the measurement of blood lactate levels is useful in the diagnosis and evaluation of hypoxia and lactic acidosis in patients in shock or with heart failure.48,49There are studies in the literature that investigated the significance of intraoperative changes in lactate levels. Their findings showed that such changes are associated with worse short-term outcomes in patients after cardiac surgery with cardiopulmonary bypass.50There are also studies that have found that there is a correlation between an increase in lactate levels in sweat and application of loads.51Those studies suggest that more research is needed into this association as lactate levels have the potential to act as a biomarker for the development of pressure ulcers.51–53In light of the known mechanism underlying pressure ulcer formation, involving ie reduced tissue perfusion, and the fact that lactate levels increase when the supply of oxygen is reduced, the significance of elevated lactate levels as a potential biomarker for pressure ulcer development should be further investigated. The incidence of pressure ulcers in patients admitted to intensive care units ranges between 3.3% and 52.9%.54A study by Sayar et al shows a PU prevalence of 14.3% in Intensive Care Unit patients at Waterlow’s risk group. This study indicates the involvement of long hospitalization and inactivity in the development of PU.55A systematic review and meta-analysis of 35 studies by Borojeny et al show that the worldwide prevalence of pressure ulcers in hospitalized patients is 12%,3however, studies in the United States estimate a prevalence from 8 to 40%.56The incidence of PU at the Department of Anesthesiology of the 4th Military Teaching Hospital in Wroclaw shown in this study (8.8%) does not differ from the results presented in the literature and is similar to the results of the European population. Despite the lack of proof of an association between elevated lactate levels and the occurrence of PU due to a too-small study group, it is suggested that this cause should be taken into consideration. At this point, it is not possible to compare the results with available data as no studies were found on this topic. The present study did not confirm an association between pressure ulcer development and lactate levels measured by arterial blood gas analysis. Although our study group was sufficiently large, the expected values were low due to the division of the groups studied into small subgroups. Therefore, we suggest that the findings from the study should be interpreted with caution. We would encourage that further research covering a much longer time period and enabling the collection of data relating to more than 1000 patients be conducted into the association between lactate levels and pressure ulcer formation in order to confirm or refute the hypothesis in question. Medical publications have reported findings that confirm an association between reduced albumin levels and increased blood lactate levels in patients after surgery. There are also many studies investigating the prognostic significance of lactate levels in the perioperative period or the behaviour of serum lactate levels in patients undergoing mechanical ventilation.29,52,57However, we found no studies in which lactate levels were identified as a risk or prognostic factor for pressure ulcer formation in patients. Our present study was motivated by the importance of pressure ulcers and the wish to identify prognostic factors for pressure ulcer development as well as the lack of scientific data that would verify the relationship between pressure ulcer formation and lactate levels. Even though our study did not confirm the association in question, we believe that the issue concerned should be investigated further. We suggest that further research into the issue should take into account the fact that rapid therapeutic interventions performed in patients can mask the actual behaviour of arterial blood lactate levels in patients with pressure ulcers, which prevents the association between lactate levels and pressure ulcer formation from being fully understood. Such research could have an impact on many aspects of medical care, including care of the physical and mental health of patients, length of hospital stay, assessment of quality of care, treatment costs and prognosis for the life and health of the patient.
Study Limitations
Considering the low expected values due to the small number of patients included in each subgroup, the findings from the study should be treated with caution. Given the importance of the issue of pressure ulcers in patients, a larger population study covering a longer period of time seems warranted.
Conclusions
The present study did not show a direct correlation between the patients’ arterial blood lactate levels and the incidence of pressure ulcers. The incidence of pressure ulcers in ICU patients is not different from the incidence rates reported in the literature. Considering the low expected values due to the small number of patients in each subgroup, the findings should be treated with caution. Given the importance of pressure ulcers, a larger population study covering a longer period of time seems warranted.
