Indirect methods of measuring blood pressure, such as Doppler ultrasonography and oscillometric measurement, are used more frequently in small animal practices than is direct arterial placement. Doppler ultrasonography blood pressure measurement (Figure 4) using a sphygmomanometer is preferred in cats and small dogs (< 10 kg [~22 lb]). Oscillometric measurement involves use of equipment that automatically inflates and deflates a cuff to determine blood pressure continuously. This is probably the easiest of all the blood pressure monitoring options.
Some veterinary practices may be intimidated by the cost of equipment needed to measure blood pressure via direct arterial catheter placement. However, the equipment required to determine mean arterial pressure alone is inexpensive compared with equipment for indirect oscillometric measurement. In addition, arterial catheters can be used to collect samples for blood gas analysis, which can provide valuable information, especially in patients with respiratory compromise.
Regardless of which method you choose, keep in mind that a single reading is not used to determine treatment; instead, we look at trends in blood pressure readings. Also, remember that the placement of the cuff is important. The most consistent cuff location in small patients is mid-forelimb.
For the purpose of this article, I will apply a mean arterial pressure of under 60 mm Hg to determine hypotension. If using a Doppler method, I will apply any readings of under 100 mm Hg systolic arterial pressure to describe hypotension.
Once a hypotensive trend has been identified, the next step is to work with the veterinarian to determine a course of action for correction.
Treating hypotension
There are several ways to treat hypotension once the underlying cause has been identified. First, it is important to record each patient’s preoperative heart rate to establish an average (base) resting rate for that individual. If your patient is bradycardic and hypotensive because of a decrease in heart rate, consider an intraoperative intravenous dose of glycopyrrolate (0.01 mg/kg) until the heart rate returns to an acceptable range. On the other hand, if your patient is bradycardic and hypotensive because of administration of an α2-adrenergic receptor agonist (commonly called an α-agonist), such as dexmedetomidine, consider administering a reversal drug, such as atipamezole (0.10-0.30 mg/kg IM). If your patient is hypotensive due to the vasodilating effects of anesthetic inhalant agents, consider decreasing the dose of the agents.
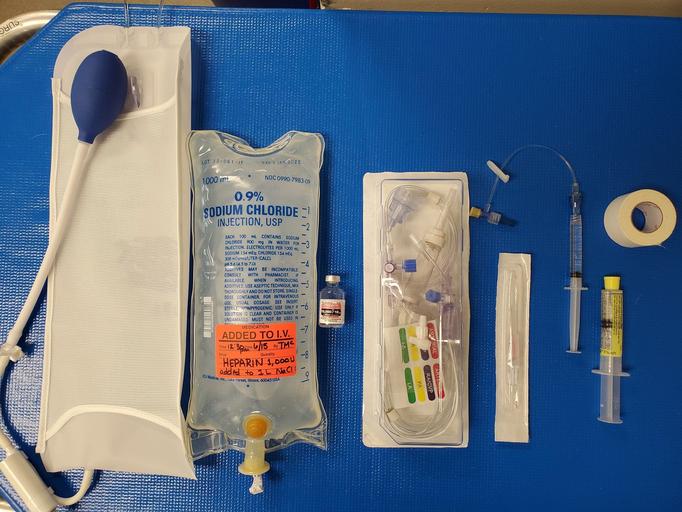
Inhalant anesthetic agents can also cause a decrease in cardiac output and, when combined with vasodilation, may lead to decreased organ perfusion. Increased circulating volume can be achieved by administering boluses (5-10 mL/kg) of intravenous crystalloid fluids, which will help if hypotension is secondary to hypovolemia and peripheral vasoconstriction. In some patients, reducing anesthetic depth and administering an increased volume of crystalloid fluids is not enough to correct hypotension. In these cases, the addition of colloids or inotropic agents should be considered. Colloidal solutions can be either natural (eg, albumin) or synthetic (eg, dextran, hydroxyethyl starch). Patients that do not respond to these treatments will need intervention with drugs to improve systemic vascular resistance and contractility. These drugs act on α- and β-adrenergic receptors. Stimulation of these receptors can have varying effects at varying doses.
Of course, before starting any therapy, talk with your clinician to verify both the drug and the dose.
Dobutamine is a synthetic catecholamine that acts on α- and β-adrenergic receptors, stimulating cardiac contractility, cardiac output, and coronary blood flow. Low doses can cause an increase in cardiac output while simultaneously initiating a moderate increase in heart rate. The therapeutic dose ranges from 2 to 20 µg/kg/min.1
Dopamine is a short-acting norepinephrine precursor with α- and β-agonist properties (ie, binds to α1-, α2-,and β2-receptors plus 2 dopamine receptors). The dosing schedule is important with this drug, as different doses can stimulate other receptors and thus trigger different effects. Medium doses (eg, 3-5 µg/kg/min) can stimulate β-adrenergic receptors that act as a positive inotrope and increase heart rate.1Higher doses (6 to 10 µg/kg/min) stimulate α-adrenergic receptors that cause an increase in systemic vascular resistance. Doses higher than 10 µg/kg/min can trigger tachycardia and increased afterload, leading to decreased cardiac output.1
Ephedrine is a noncatecholamine sympathomimetic agonist that stimulates α- and β-adrenergic receptors. Another benefit of ephedrine is improved oxygen delivery to tissues via increased hemoglobin. Ephedrine can also be administered as a single-bolus intravenous injection of 0.10 mg/kg.2
Norepinephrine acts on α- and β-receptors by increasing mean arterial pressure and peripheral vascular resistance. Coronary blood flow also increases. Norepinephrine may be beneficial in increasing mean arterial pressure in patients with sepsis or patients currently on β-blocking drugs such as atenolol.1Often, norepinephrine infusions are started at 0.10 to 0.20 µg/kg/min and can be increased by increments of 0.10 to 0.20 µg/kg/min as needed. It is important to note that norepinephrine is not usually the first choice for hypotensive patients that are otherwise healthy. It is often used in the treatment of vasodilatory shock and commonly administered with an inotrope (such as dobutamine) if myocardial depression is suspected.
References
Tasha McNerney, BS, CVT, VTS (anesthesia and analgesia), CVPP, is an author, lecturer, and administrator for Veterinary Anesthesia Nerds.
