Hypertension is a well-known risk factor for cardiovascular disease (CVD) and all-cause mortality worldwide1. Effective lifestyle modification and anti-hypertensive drug treatment strategies can reduce blood pressure (BP) in hypertensive patients2. Nevertheless, BP control rates are still poor worldwide and are not satisfactory in Korea or across Europe3. In particular, acute and severe BP elevations due to uncontrolled hypertension are serious problems commonly encountered in patients visiting the emergency department (ED). According to our previous study, patients with acute severe hypertension, which was defined as systolic blood pressure (SBP) ≥ 180 mmHg or diastolic blood pressure (DBP) ≥ 100 mmHg, accounted for 59 out of 1000 ED visits at a single center and showed poor clinical outcomes, with a 1-year mortality rate of 8.8% and a 3-year mortality rate of 13.9%4.
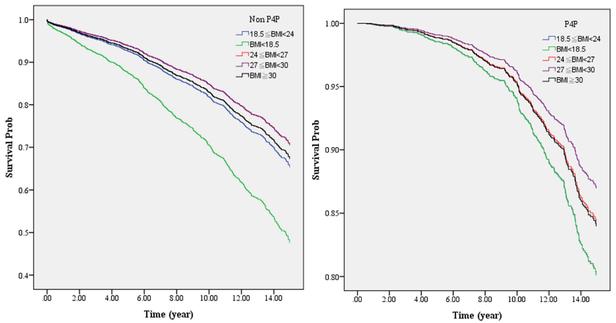
Body mass index (BMI) is one of the markers of obesity and body fat5, which has a strong association with all-cause mortality. Most studies demonstrated a J- or U-shaped association with the lowest mortality in people with an optimal BMI (20–25 kg/m2) range6,7,8,9. However, the obesity paradox implies that overweight and mildly obese groups have a better prognosis for all-cause mortality10. Low BMI (2) may be a risk factor for CVD and all-cause mortality, which may be attributed to aging, sarcopenia, and poor nutritional status in the underweight population11. Although underweight and obesity are important clinical characteristics of patients with CVD, few studies have attempted to demonstrate the effect of BMI on all-cause death or cardiovascular outcomes in patients with acute severe hypertension.
In this study, we investigated the association of BMI level with all-cause mortality during long-term follow-up in patients with acute severe hypertension who visited the ED.
