Davida Kruger, NP: I want to talk about some of the newer medications in diabetes but before we get there, can you talk to us about, what do you think about how you need to manage hypertension, number 1, that whole concept of, “My blood pressure is only high when I come see you. Do I need a medication?” and then we’ll talk about how do we control lipids. All of these things that lead up to cardiovascular disease [CVD]. Let’s start with hypertension.
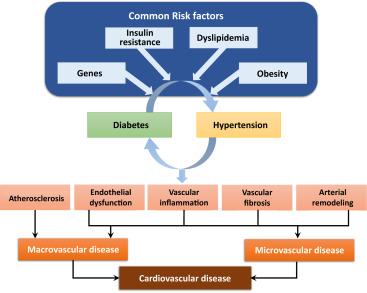
Margo B. Minissian, PhD, ACNP: Hypertension is the leading killer worldwide and drives heart disease. It links hand and hand with blood cholesterol and blood sugar and many of us learned it being described as metabolic syndrome, for example. What we’ve learned from this research is that it’s all about inflammation and that inflammation is driven by hypertension in particular and the guidelines have been in 2018, so it’s really important for men and women to understand that their blood pressure should be less than 120 over 80 all the time. Otherwise they have stage 1 hypertension with a 120 over 81 blood pressure, and lower is truly better when it comes to blood pressure.
Davida Kruger, NP:Do you recommend patients check their blood pressure at home, and if you do, how frequently and what do you do with that data?
Margo B. Minissian, PhD, ACNP: Home blood pressure monitoring is a staple and should be a staple to our patients’ regimen. The more that we can empower our patients to obtain their own data at home, or in their work environment to reflect how they are doing in their day-to-day activities is powerful. Andhaving them do random checks, I feel is an important piece of it, especially if they are on medications. You know we’ve taught different ways of being able to measure blood pressure at home but depending on what time of day a patient is choosing to measure their blood pressure, has a lot to do with the way that they measure their blood pressure at home. Teaching a patient to sit firmly in a chair, having both feet on the floor, having their arm up maybe on a pillow or side of a sofa, putting a validated type of a blood pressure monitor on their arm, and then the hardest part for most people is to sit and try to relax for 3 to 5 minutes before they press the button. And not to be texting or talking or answering phones or emails while they’re doing it, to truly give themselves a baseline blood pressure. That is an important education piece that we share with our patients.
Davida Kruger, NP: One of the things I started doing in the clinic, and I actually did it last week because a patient came in rushing from the parking lot, sat down, bless their hearts, the MA’s [medical assistant’s] do the best they can but they’re time constrained and I got this horrible blood pressure on this patient who had been well-controlled on the medications I prescribed. I do this frequently. I took the patient back out, made sure the right cuff, the right size cuff, and she said, “Well that wasn’t the cuff that was used on me before.” I said, “This is the cuff you should always use,” put the cuff on, showed her how it was supposed to be fitted, made her put her feet on the ground and I said give me your phone and I said “I’m going to step away, around the corner for 3 to 5 minutes and you’re not allowed to talk to anybody.” I came back, did her blood pressure, and it was beautiful and I said, “Here’s the thing, if you come into my office or any health care providers office, it’s OK to say can you do this, and this is how to get a good blood pressure,” because if we educate them at home and they bring it into the practice, then we’re going to get much better. Plus, if they had done it right I would’ve saved about 20 minutes of my time. But I do try to educate my patients so that they do get a good blood pressure with a good blood pressure cuff.
Margo B. Minissian, PhD, ACNP: That’s absolutely the case, and if you as a clinician are scratching your head and you’re not sure that the numbers you are seeing are accurate at home or whether you’re seeing accurate numbers in the office, the gold standard for blood pressure measurement and diagnosis is an ambulatory blood pressure monitor. Remember that we have that, and especially if you are trying to rule out white coat hypertension, if you’re trying to get the ambulatory blood pressure monitor paid for by insurance it’s important that we are appropriately labeling these with the correct ICD-10 codes as well. That is truly the gold standard, otherwise we are seeing elevations in clinic, 30% of the time you’re seeing elevations at home and 30% of the time you are seeing normal pressures at home and the office. Those numbers don’t look that great. The more we teach people to do it appropriately is best because we are not rocks, we are not inanimate object. If we’re upset, if we’re running, you need your blood pressure to elevate, that’s our flight or fight mode and you have to control for it with standardization of measurement.
Davida Kruger, NP: Outstanding, thank you. Those are great tips and the things that we need to teach our patients so that they are comfortable with it as well. Sometimes I also have my patient bring their home reader in and have them do a blood pressure after we’ve got a good blood pressure in the office to make sure it’s still calibrated.
I want to thank our audience for watching HCPLive® Peers and Perspectives. If you enjoyed the content, please subscribe for our new e-newsletter to receive upcoming Peers and Perspectives and other great content right in your inbox. I receive it and I really love it when I see it in there. Take some time to enjoy it. Thank you again for joining us.
